What To Know About Osteoporosis and Lower Back Ache
Understanding Osteoporosis and Its Impact on Lower Back Ache
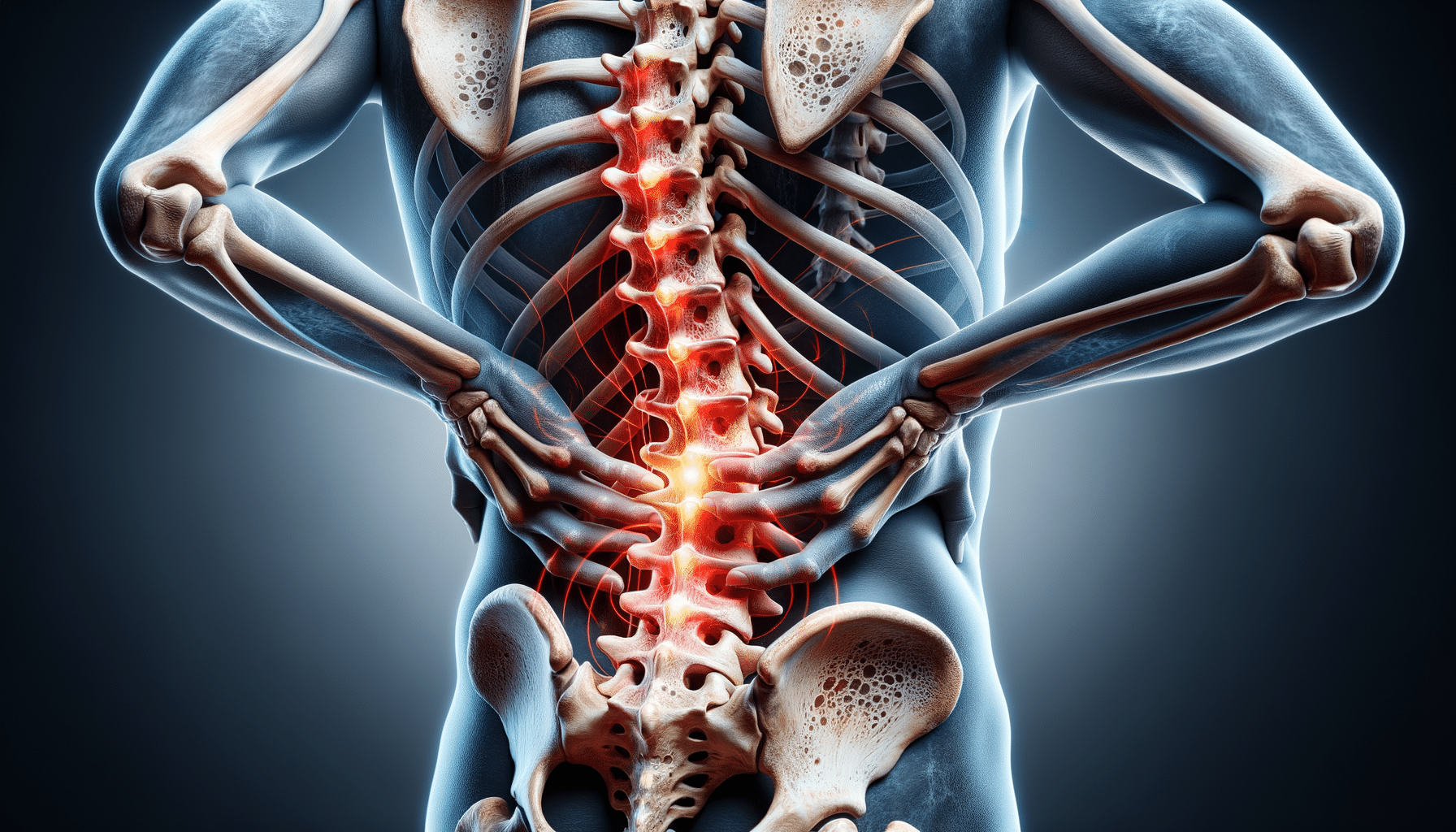
Osteoporosis, a condition characterized by weakened bones, poses significant health challenges, particularly as individuals age. It often goes unnoticed until a fracture occurs, making it a silent threat. Among the various complications associated with osteoporosis, lower back ache is a prominent concern. The spine, a crucial support structure for the body, is composed of vertebrae that are particularly vulnerable to bone density loss. As osteoporosis progresses, these vertebrae can become fragile, leading to fractures or compression, which subsequently results in pain and discomfort.
The lower back, or lumbar region, is especially susceptible to these changes. As the vertebrae weaken, they may collapse, leading to a stooped posture and reduced height. This not only affects physical appearance but also contributes to chronic pain. The pain can range from mild discomfort to severe, debilitating aches that interfere with daily activities. Understanding this connection between osteoporosis and lower back ache is crucial for managing symptoms and improving quality of life.
Several factors contribute to the onset of osteoporosis, including age, hormonal changes, and lifestyle choices. Women, particularly post-menopausal women, are at a higher risk due to the decrease in estrogen levels, which plays a vital role in maintaining bone density. Therefore, addressing these factors through lifestyle modifications and medical interventions can help mitigate the impact of osteoporosis on the lower back.
Normal Bone Density for a 70-Year-Old Woman
Bone density is a critical measure of bone health, reflecting the strength and structural integrity of bones. For a 70-year-old woman, maintaining bone density is essential to prevent fractures and other complications associated with osteoporosis. Bone density is commonly assessed using a test called a Dual-Energy X-ray Absorptiometry (DEXA) scan, which provides a T-score indicating how much one’s bone density deviates from the norm for a healthy young adult.
For a 70-year-old woman, a T-score between -1 and -2.5 suggests osteopenia, a condition of lower-than-normal bone density that precedes osteoporosis. A T-score of -2.5 or lower indicates osteoporosis. While these scores provide a general guideline, individual bone health can vary based on genetics, lifestyle, and medical history.
Maintaining bone density involves several strategies, including adequate calcium and vitamin D intake, regular weight-bearing exercises, and lifestyle modifications such as quitting smoking and limiting alcohol consumption. These measures can help slow bone loss and maintain bone strength, reducing the risk of fractures and associated lower back pain.
Regular monitoring of bone density is essential for early detection and management of osteoporosis. Women over the age of 65 are generally advised to undergo bone density testing every two years, though those with risk factors may need more frequent assessments. By understanding and monitoring bone density, women can take proactive steps to maintain their bone health and overall well-being.
Managing Osteoporosis: Medication and Reversibility
When it comes to managing osteoporosis, medication plays a crucial role in slowing bone loss and reducing fracture risk. Various medications are available, each working through different mechanisms to enhance bone strength. These include bisphosphonates, which slow down bone resorption, and selective estrogen receptor modulators (SERMs), which mimic estrogen’s bone-protective effects. Additionally, newer treatments like monoclonal antibodies target specific pathways involved in bone turnover.
While medication is effective in managing osteoporosis, it is not the sole solution. Lifestyle changes, such as a balanced diet rich in calcium and vitamin D, regular exercise, and fall prevention strategies, are equally important. These measures complement medication by addressing the root causes of bone loss and enhancing overall bone health.
A common question is whether osteoporosis can be reversed. While significant bone loss cannot be fully restored, the progression of osteoporosis can be halted or slowed with appropriate treatment. In some cases, bone density can be improved to a certain extent, especially with early intervention. This underscores the importance of regular bone density monitoring and timely treatment initiation.
Ultimately, managing osteoporosis requires a comprehensive approach that combines medication, lifestyle changes, and regular medical check-ups. By understanding the available treatment options and taking proactive steps, individuals can effectively manage osteoporosis and maintain their quality of life.