Ways to Help Prevent Pressure Sores in Bedridden Elderly
Is skin integrity a concern for those with limited mobility? Maintaining healthy tissue requires diligent attention and proactive measures. Understanding preventative approaches is crucial for individuals providing care.
Understanding Pressure Sores
Pressure sores, also known as bedsores or decubitus ulcers, are injuries to the skin and underlying tissue resulting from prolonged pressure on the skin. They often develop on skin covering bony areas of the body, such as the heels, ankles, hips, and tailbone. For individuals with limited mobility, such as the elderly who are bedridden, these sores can pose a significant health risk.
The development of pressure sores is a complex process involving several factors. Key contributors include sustained pressure, shear, friction, and moisture. When pressure is applied to the skin for extended periods, it restricts blood flow, depriving tissues of oxygen and nutrients. This can lead to tissue damage and the formation of sores.
Understanding the stages of pressure sores is crucial for early detection and treatment. They range from Stage 1, where the skin is intact but red and may be warm to the touch, to Stage 4, which involves deep tissue damage, potentially reaching muscles and bones. Recognizing these stages helps caregivers take appropriate actions to prevent further deterioration.
To combat the development of pressure sores, it is essential to implement a comprehensive care plan that includes regular assessment and monitoring. This ensures that any early signs of pressure sores are identified and addressed promptly, reducing the risk of severe complications.
Implementing Preventive Strategies
Preventing pressure sores requires a proactive approach that involves multiple strategies. For caregivers, understanding these strategies is vital to maintain the skin integrity of those in their care. Regular repositioning is one of the most effective methods. By shifting the position of bedridden individuals at least every two hours, caregivers can alleviate sustained pressure on vulnerable areas.
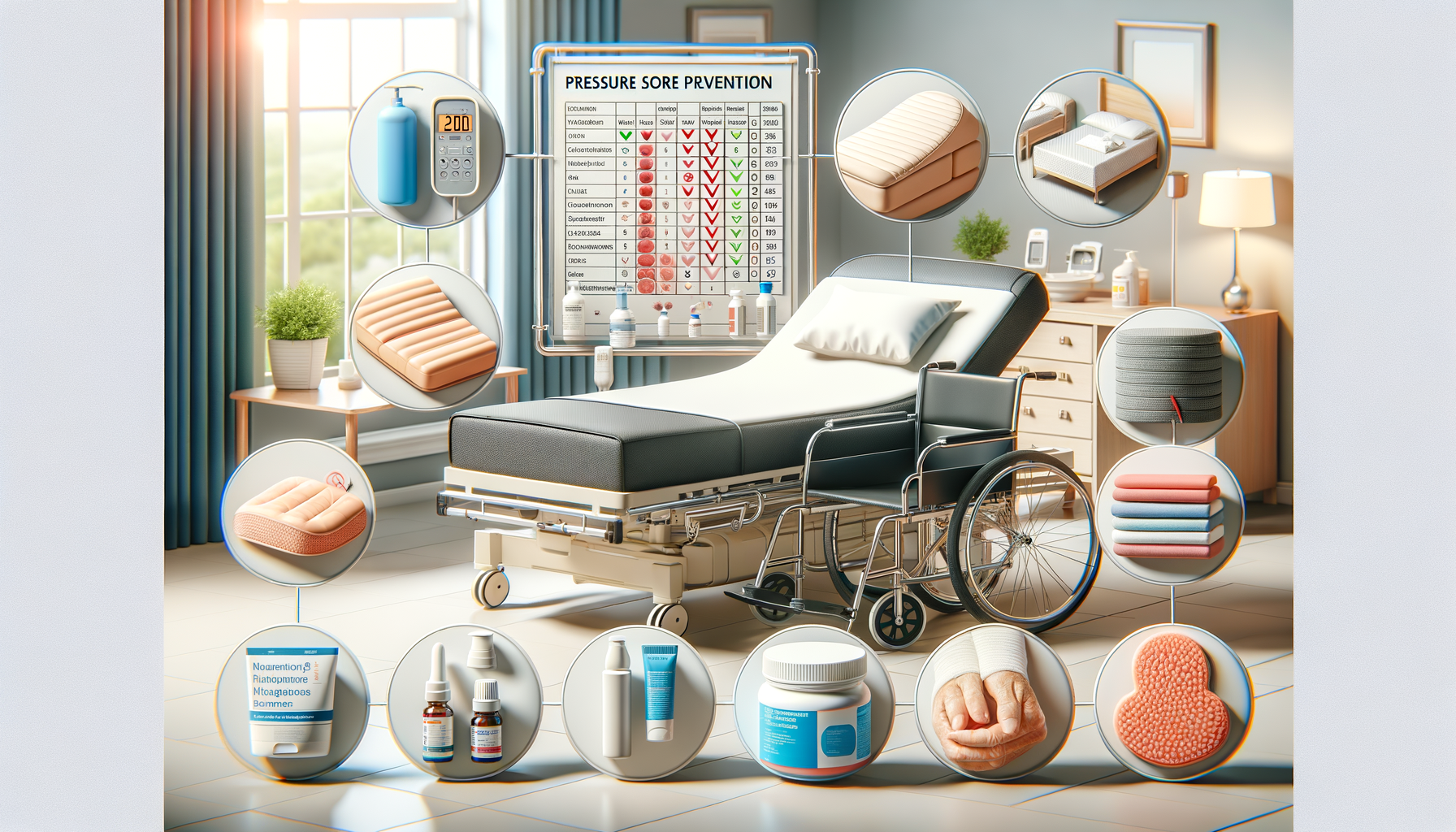
Utilizing specialized support surfaces such as foam mattresses, air-filled cushions, or gel pads can also play a critical role in prevention. These surfaces help distribute weight evenly and reduce pressure points. Additionally, ensuring that bed linens and clothing are smooth and free from wrinkles can minimize friction and shear forces that contribute to skin breakdown.
Nutrition and hydration are fundamental components of skin health. A balanced diet rich in vitamins and minerals supports tissue repair and enhances the skin’s resilience. Proper hydration helps maintain skin elasticity and prevents dryness, reducing the risk of sores.
Implementing a skincare routine that includes gentle cleansing and moisturizing can further protect the skin. Using pH-balanced cleansers and applying moisturizer can prevent skin from becoming dry and fragile, which is more susceptible to damage.
Daily Care and Monitoring
Daily care and monitoring are crucial elements in the management of pressure sores. Regular skin inspections should be part of the daily routine for individuals at risk. Caregivers should pay close attention to areas prone to pressure sores, checking for signs of redness, warmth, or swelling.
Maintaining a detailed record of skin assessments can help track changes over time and provide valuable information for healthcare professionals involved in the care plan. This documentation can guide adjustments in care strategies as needed to prevent the progression of sores.
In addition to physical care, educating both caregivers and patients about the risks and prevention strategies for pressure sores is essential. Awareness and understanding empower individuals to take an active role in their care, promoting better outcomes.
Caregivers should also be trained in recognizing signs of infection, such as increased pain, redness, or drainage from a sore. Early intervention can prevent complications and promote healing, emphasizing the importance of vigilance in daily care routines.
Ultimately, a collaborative approach involving caregivers, healthcare professionals, and patients is key to effectively managing and preventing pressure sores. This teamwork ensures that all aspects of care are addressed, providing the best possible outcomes for those at risk.