What Arthritis Does To Hip Pain and How To Address It
Could a persistent ache in the hip signal something more? Understanding the potential connection between joint discomfort and the effects on mobility can offer valuable insights. Exploring how certain conditions might impact the hip joint is a key step in seeking clarity.
Understanding Arthritis in the Hips
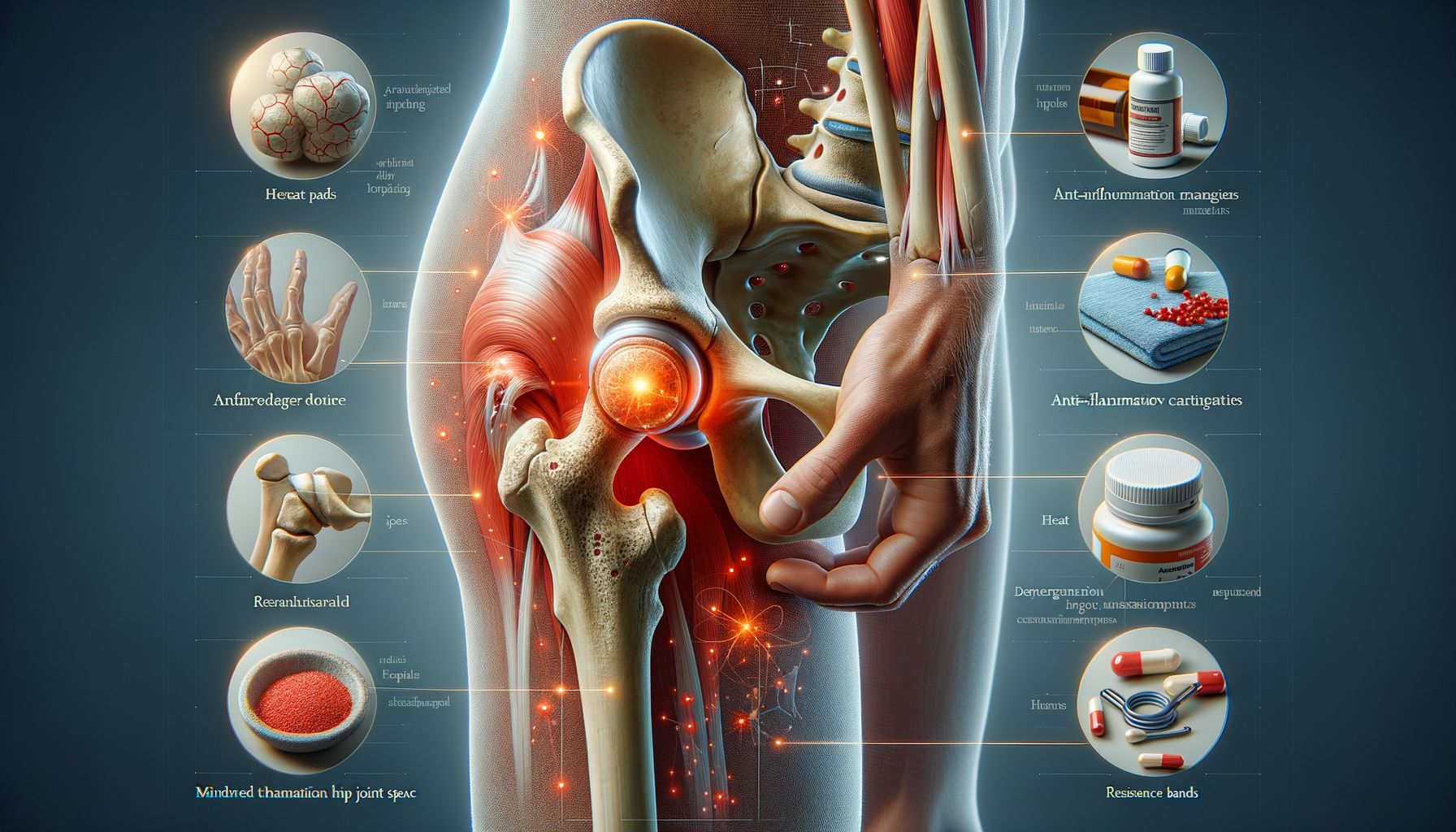
Arthritis in the hips is a condition that affects millions of people worldwide, often leading to significant discomfort and reduced mobility. The hip joint, a ball-and-socket joint, plays a crucial role in supporting the body’s weight and enabling a wide range of motion. When arthritis affects this joint, it can lead to pain and stiffness, making everyday tasks challenging. There are several types of arthritis that can impact the hip, with osteoarthritis being the most common. This degenerative joint disease results from the wear and tear of cartilage, the protective tissue at the ends of bones. As the cartilage deteriorates, bones can rub against each other, causing pain and inflammation.
Rheumatoid arthritis is another type that can affect the hips. It is an autoimmune disease where the body’s immune system mistakenly attacks the joint lining, causing inflammation and joint damage. While less common, ankylosing spondylitis, a form of arthritis that primarily affects the spine, can also involve the hip joints, leading to stiffness and pain. Understanding the type of arthritis affecting the hip is crucial for effective management and treatment.
Recognizing the early signs of hip arthritis can lead to timely intervention and better outcomes. Individuals may notice a gradual onset of pain, often described as a deep ache in the groin or buttocks. This pain can worsen with activity and improve with rest. Stiffness, especially in the morning or after sitting for long periods, is another common symptom. As the condition progresses, individuals may experience reduced range of motion, making it difficult to bend over or put on shoes. Swelling and tenderness around the hip are also possible indicators of arthritis.
Recognizing Symptoms of Hip Arthritis
Identifying the symptoms of hip arthritis early can make a significant difference in managing the condition effectively. One of the most common signs is persistent pain in the hip joint, which can radiate to the groin, thigh, or buttocks. This pain often intensifies with physical activity and may be accompanied by a sensation of grinding or clicking in the hip. Morning stiffness is another hallmark symptom, typically easing with movement as the day progresses.
In addition to pain and stiffness, individuals may notice a decreased range of motion in the hip joint. This can manifest as difficulty performing everyday activities such as walking, climbing stairs, or bending down. Over time, the joint may become increasingly swollen and tender to the touch, signaling inflammation. A noticeable limp or change in gait can also develop as the body compensates for the discomfort.
It’s important to note that the severity and progression of symptoms can vary widely from person to person. Some individuals may experience mild discomfort that comes and goes, while others may face chronic pain and significant limitations in mobility. Consulting with a healthcare professional for a proper diagnosis and tailored treatment plan is essential for managing hip arthritis effectively.
Effective Management Strategies for Arthritic Hip Pain
Managing arthritic hip pain effectively requires a comprehensive approach that addresses both symptoms and underlying causes. Lifestyle modifications, such as maintaining a healthy weight, can significantly reduce stress on the hip joints. Regular low-impact exercises, like swimming or cycling, help maintain joint flexibility and strengthen surrounding muscles, providing better support for the hip joint.
Physical therapy is another valuable tool in managing hip arthritis. A physical therapist can design a personalized exercise program to improve range of motion and strengthen the muscles around the hip. They may also recommend assistive devices, such as canes or walkers, to alleviate pressure on the joint and enhance mobility.
Medication can play a crucial role in managing pain and inflammation. Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can provide relief for mild to moderate pain. For more severe cases, a healthcare provider may prescribe stronger medications or recommend corticosteroid injections to reduce inflammation.
In cases where conservative treatments are insufficient, surgical options may be considered. Hip replacement surgery, where the damaged joint is replaced with an artificial one, can offer significant pain relief and improve function. However, surgery is typically reserved for individuals who have not found relief through other means and are experiencing a considerable impact on their quality of life.
Ultimately, the key to managing arthritic hip pain lies in a tailored approach that considers the individual’s specific needs and lifestyle. Regular consultations with healthcare providers ensure that the management plan remains effective and adaptable to any changes in the condition.