What To Know About Antidepressant Risks for Seniors Over 80 With Mild Depression
Could a common treatment option carry unique considerations for an aging population? For individuals navigating later life with mood changes, understanding the potential effects of certain medications becomes important. Exploring the nuances surrounding antidepressant use in those over 80 with mild depression offers valuable insights.
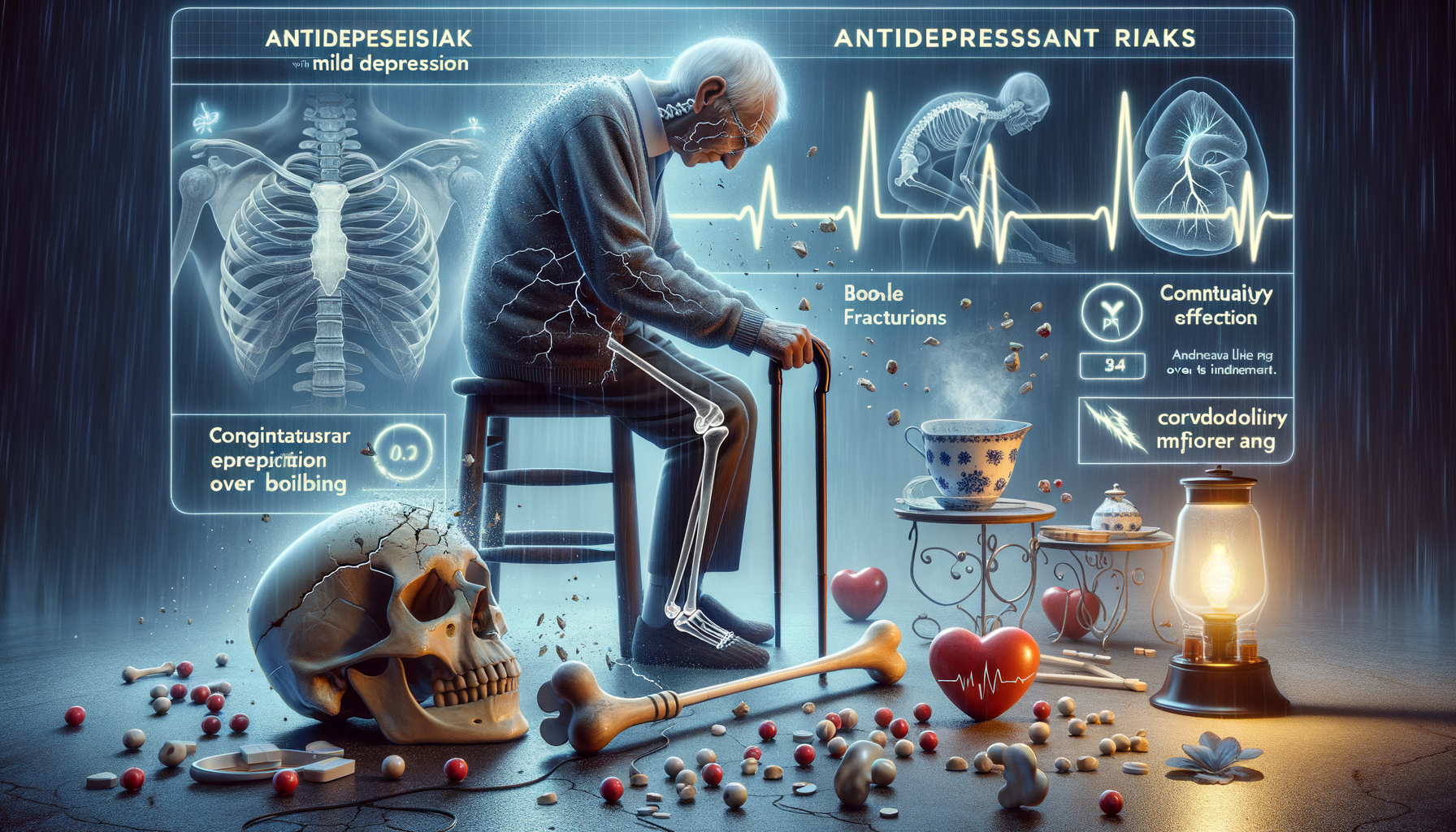
Increased Fall Risk and Bone Fractures
As individuals age, the risk of falls and subsequent bone fractures naturally increases. This risk is further amplified in seniors over 80 who are prescribed antidepressants for mild depression. Antidepressants can affect balance and coordination, leading to an increased fall risk. This is particularly concerning for older adults, whose bones may be more fragile and susceptible to fractures.
Several factors contribute to this increased risk. Firstly, certain antidepressants can cause dizziness or sedation, both of which can impair physical stability. Secondly, the presence of other health conditions common in the elderly, such as arthritis or vision problems, can exacerbate balance issues. Thirdly, interactions with other medications can further complicate the situation, potentially leading to side effects that increase fall risk.
To mitigate these risks, it is essential to monitor the elderly closely when they begin antidepressant treatment. Regular assessments by healthcare professionals can help identify any adverse effects early on. Additionally, implementing safety measures in the home, such as removing tripping hazards and installing grab bars, can significantly reduce fall risk.
- Regular exercise to improve strength and balance
- Vision checks to ensure optimal eyesight
- Medication reviews to avoid harmful interactions
By addressing these factors, the potential for falls and fractures can be minimized, allowing seniors to maintain their independence and quality of life.
Cognitive Impairment and Dementia Concerns
Cognitive impairment and dementia are significant concerns for seniors, particularly when antidepressants are involved. While these medications are designed to improve mood and mental health, they can sometimes have unintended effects on cognitive functions. This is especially true for older adults who may already be experiencing age-related cognitive decline.
Research indicates that some antidepressants can affect neurotransmitter levels in the brain, which may contribute to cognitive changes. Symptoms such as confusion, memory lapses, and difficulties with concentration can arise, potentially mimicking or exacerbating dementia-like symptoms. For seniors over 80, who may already be at a higher risk for conditions like Alzheimer’s disease, this is a critical concern.
To address these issues, it is crucial for healthcare providers to conduct thorough cognitive assessments before and during antidepressant treatment. This allows for the early detection of any cognitive side effects, enabling timely intervention. Family members and caregivers should also be informed about the potential risks and encouraged to report any noticeable changes in cognitive function.
- Engaging in cognitive activities to stimulate the brain
- Maintaining a healthy diet rich in brain-boosting nutrients
- Ensuring adequate sleep and stress management
By taking these proactive steps, the potential cognitive impact of antidepressants on seniors can be managed more effectively, preserving mental acuity and overall well-being.
Cardiovascular Effects and Monitoring
The cardiovascular system is another area of concern when it comes to antidepressant use in seniors over 80. Some antidepressants have been associated with cardiovascular effects, such as changes in heart rate and blood pressure. For seniors, who may already have underlying heart conditions, this can pose a significant health risk.
Cardiovascular effects can vary depending on the type of antidepressant prescribed. For instance, certain medications may cause an increase in heart rate, while others could lead to hypotension. These effects can be particularly dangerous for older adults, who may have less resilient cardiovascular systems.
To mitigate these risks, regular cardiovascular monitoring is essential. This includes routine blood pressure checks and heart rate assessments. Healthcare providers should also be vigilant in reviewing the patient’s overall medication regimen to avoid potential interactions that could exacerbate cardiovascular issues.
- Adopting a heart-healthy diet rich in fruits, vegetables, and whole grains
- Engaging in regular physical activity suitable for their fitness level
- Avoiding smoking and limiting alcohol consumption
By implementing these lifestyle changes and maintaining close communication with healthcare providers, seniors can better manage the cardiovascular effects of antidepressants, ensuring safer and more effective treatment outcomes.